How Body-Based Therapy (Polyvagal + ACT) Helps You Heal from Trauma
Why trauma lives in the body, not just the mind
Have you ever felt like your body was reacting way more intensely than the situation called for? Maybe your heart was racing, you felt numb, or you couldn’t speak, even though there was no imminent danger? That’s often a sign of nervous system dysregulation.
When we go through chronic trauma or stress, our body’s natural survival system can get stuck in overdrive. It’s trying to keep us safe, so let’s try to offer gentleness and compassion to that part of ourselves. Instead of turning off when the threat is gone, it keeps firing, leaving us on edge or shut down.
Understanding the four survival responses
Fight
You feel angry, reactive, and at the ready. Your body is preparing to protect you.
"Why did they say that? Oh man, it’s on."
Flight
You feel anxious or restless. You might leave a situation or distract yourself.
"I’m out of here!"
Freeze
You feel numb, stuck, or disconnected.
"It’s like I’m not even here."
Fawn
You feel a strong need to please others to avoid conflict, even at your own expense.
"If I keep them happy, maybe I’ll be safe."
These are normal protective responses, especially if you’ve lived through trauma or ongoing stress. But when they get stuck “on,” they can interfere with relationships, decision-making, and your overall sense of safety.
They also show up in the body:
Fight or flight might cause you to tighten your jaw or tense your shoulders
Freeze might feel like being weighed down or chronically fatigued
Fawn might come with physical tension or never fully feeling at rest, even when alone
Why does trauma stay in the body?
Trauma is stored through sensory memory and nervous system wiring. If we weren’t able to move, cry, speak, or process an experience safely, the body may hold onto that unexpressed energy. You can think of it like a record stuck on replay. And there’s hope! Keep reading…
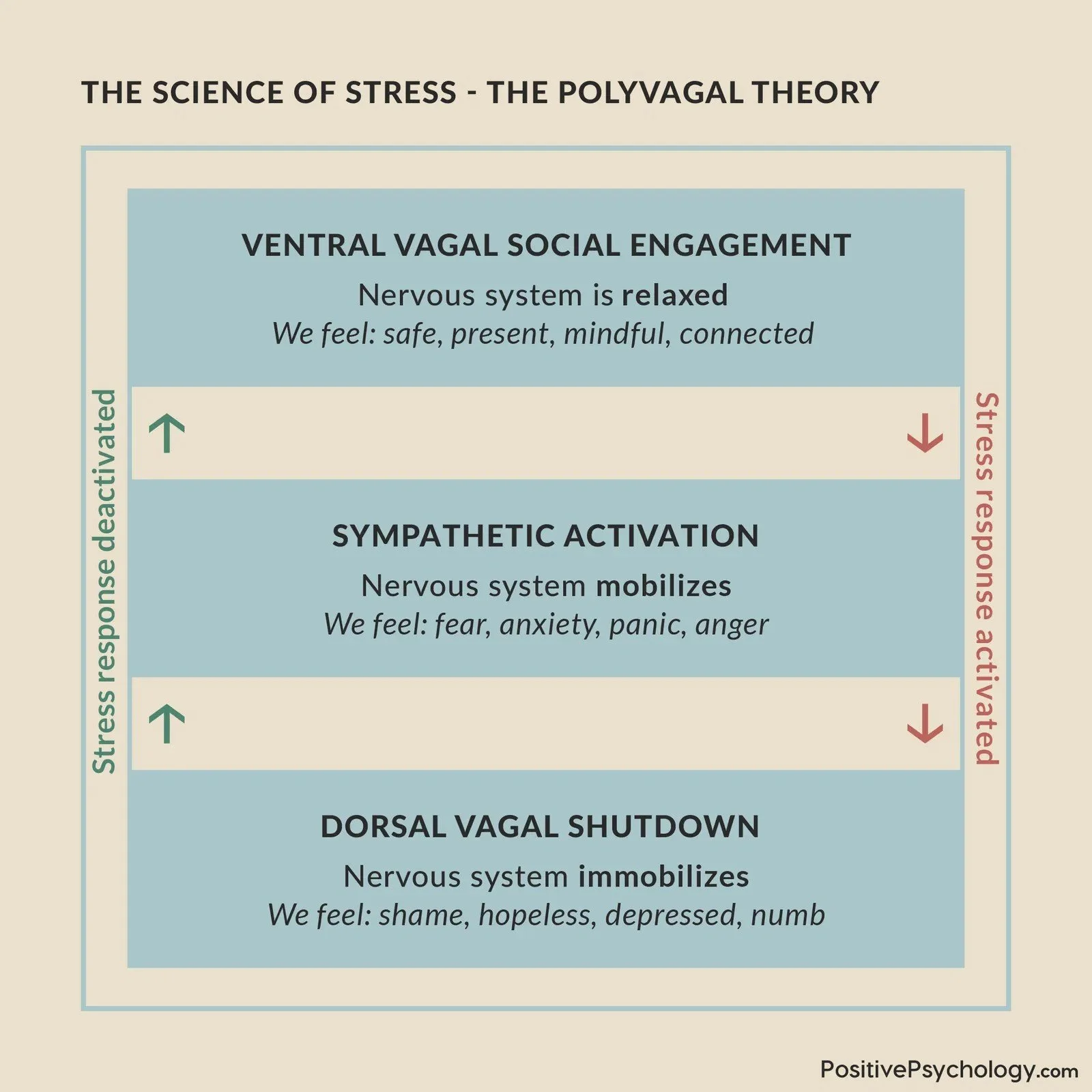
What is Polyvagal Theory?
Developed by Dr. Stephen Porges, Polyvagal Theory helps us understand how the vagus nerve monitors safety and danger in our environment. The dorsal vagal branch of the nerve triggers shutdown or freeze states. Chronic trauma can interfere with healthy activation of this system, affecting our capacity to feel calm, connected, and emotionally regulated.
The 3 main nervous system states in our bodies…
1. Ventral vagal – when we feel safe, calm, and connected
2. Sympathetic – fight or flight activation
3. Dorsal vagal – shutdown or freeze under extreme threat
Trauma can disrupt this system, leaving us more reactive, prone to dissociation and shutdown.
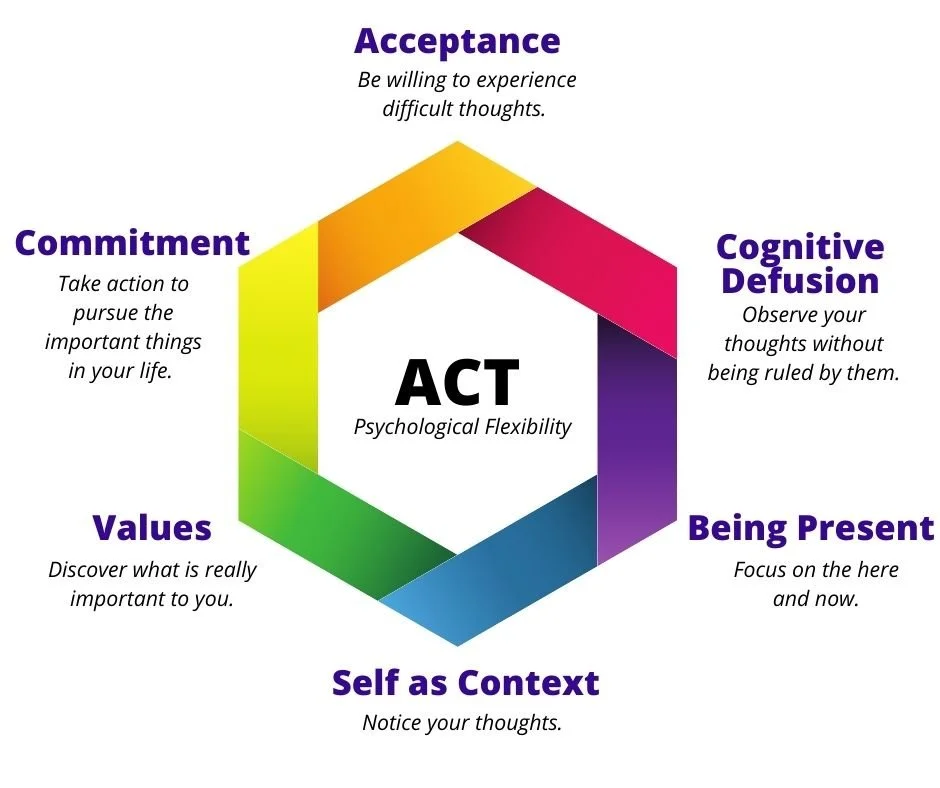
What Is Acceptance and Commitment Therapy?
Developed by Dr. Steven Hayes, ACT blends mindfulness, acceptance, and values-driven action. It helps people live more meaningfully even when difficult thoughts or emotions are present. Core processes include:
Present-moment awareness
Cognitive defusion (creating space from thoughts)
Committed action (aligning behaviour with personal values)
ACT builds psychological flexibility, which supports emotional resilience and growth.
When you can’t think your way out of it
When your nervous system is stuck in survival mode, it’s hard for your brain to think clearly or make helpful decisions.
That’s because dysregulation affects key brain areas:
The amygdala (our alarm system) becomes overactive, triggering a sense of urgency
The prefrontal cortex (our decision-maker) becomes less active, making it harder to problem-solve or reflect
Polyvagal Theory teaches us how to support nervous system healing by creating safety in the body through grounding, movement, and somatic awareness. Once our system shifts toward safety, ACT tools tend to become more accessible and effective.
Where Polyvagal Theory and ACT meet
Regulation first, action second
So why do these two approaches work so well together? Polyvagal Theory offers a bottom-up approach. It starts with the body and builds a felt sense of safety. ACT brings a top-down lens. It supports meaningful action and mental flexibility once there’s enough nervous system regulation in place.
Here’s a common scenario: you try to do something brave (like speak up in a meeting or go on a date) and suddenly your mind floods with thoughts like:
"They’ll reject you."
"This is going to go badly."
In ACT, we often use a metaphor: You are the driver of a bus, and those thoughts are just passengers. They might be loud, but they don’t get to steer. But if your body doesn’t feel safe, if your nervous system is in fight, flight, freeze, or fawn, the metaphor might not be enough. You might feel shut down or emotionally hijacked. That’s your body doing its best to protect you.
What to do when feeling shut down or emotionally hijacked
Before trying to “drive,” try anchoring in your body first:
Feel your feet on the floor
Take a long, slow breath
Notice one small point of safety or support in your environment
These small actions help your nervous system shift toward connection. Polyvagal Theory calls this the ventral vagal state. Once your body feels a bit steadier, you can return to the metaphor. Those thoughts might still be there, but now you can notice them from the driver’s seat without letting them take the wheel. You can move forward without needing to push through.
Trauma-informed ACT
Blending body awareness and gentle action
In trauma-informed ACT, we blend body awareness with gentle, meaningful action. You don’t have to silence your mind or override your body.
Instead, you can learn to:
Listen to your body’s cues
Stay grounded in the present
Choose your direction with care and intention
Change is possible when the body feels safer
Trauma lives in the body. Healing comes through body-mind integration, as we’ve just gently explored together. Progress is possible through flexibility, compassion, and body-informed trauma therapy. If this resonates and you’re curious about working with a therapist who offers Polyvagal-informed ACT and somatic therapy for anxiety or trauma, our team would be honoured to support you.
Complete our Meet Your Match form to be connected with an experienced therapist in person at our office in the Riverdale community of East York, Toronto, and online across Ontario.
Gentle body-based exercises to support nervous system regulation
Regulation is a practice. It’s okay if it takes time to feel comfortable doing it.
Grounding With Your Feet
Place your feet flat on the floor beneath you
Notice the sensation of your feet touching the ground
Gently press your feet down and feel the support beneath you
Take three slow, deep breaths while keeping your attention on your feet
Hand-on-Heart
Place your right hand on your heart
Close your eyes, if comfortable
Notice your heartbeat and the rise and fall of your chest
Breathe softly, allowing a sense of gentleness and safety to grow
References
Polyvagal Theory and How It Relates to Social Cues – Verywell Mind
Polyvagal Theory: An Approach to Understanding Trauma – Psychology Today
Polyvagal Theory Explained (and 18 Exercises) – PositivePsychology.com
What is Acceptance and Commitment Therapy? – Thrive Training Consulting
Van der Kolk, B. (2015). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. Penguin Books
When the Body Remembers – Psychology Today